Best Medical coding Training center In Trivandrum
N42.31
Prostatic intraepithelial Neoplasia
Prostatic intraepithelial neoplasia (PIN) is a condition “defined by neoplastic growth of epithelial cells within preexisting benign prostatic acini or ducts.” Because PIN satisfies almost all the requirements for a premalignant condition, high-grade PIN (HGPIN) is widely accepted as a precursor to prostate cancer.
High-grade prostatic intraepithelial neoplasia is considered the most likely precursor of prostatic carcinoma. The only method of detection is biopsy; prostatic intraepithelial neoplasia (PIN) does not significantly elevate serum prostate-specific antigen concentration and cannot be detected by ultra-sonography. The incidence of PIN in prostate biopsies averages 9% (range, 4%–16%), representing 115,000 new cases of PIN diagnosed each year in United States. PIN has a high predictive value as a marker for adenocarcinoma, and its identification warrants repeated biopsy for concurrent or subsequent invasive carcinoma. Carcinoma will develop in most patients with PIN within 10 years. PIN is associated with progressive abnormalities of phenotype and genotype that are intermediate between normal prostatic epithelium and cancer, indicating impairment of cell differentiation and regulatory control with advancing stages of prostatic carcinogenesis. Androgen deprivation therapy decreases the prevalence and extent of PIN, suggesting that this form of treatment may play a role in chemoprevention.
Prostatic intraepithelial neoplasia (PIN) represents the preinvasive end of the continuum of cellular proliferations within the lining of prostatic ducts and acini. The term “PIN” is usually used today as a synonym for high-grade PIN (HGPIN) (formerly PIN grades 2 and 3 on a 1–3 scale). The high level of interobserver variability with low-grade PIN limits its clinical utility, and pathologists do not routinely report this finding except in research studies.1 Interobserver agreement for HGPIN is “good to excellent.”Other terms, such as “dysplasia,” “carcinoma in situ,” and “intraductal carcinoma,” are discouraged.
Prostatic Intraepithelial Neoplasia (PIN)
- Generally regarded as probable precursor lesion for prostate carcinoma.
- Divided into low grade (mild dyplasia) and high grade Prostatic Intraepithelial Neopplasia (HGPIN, severe dysplasia).
- HGPIN is detected in 80-100% of prostate harboring carcinoma.
- Like in prostate cancer, TMPRSS-ERG fusion is also detected but at a lower rate in HGPIN (19%) than prostate cancer (~50%).
- Histology:
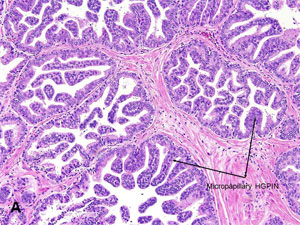
- Preexisting (non-invasive) ducts and acini, usually medium to large size, lined by crowded cells with abnormal cytologic features (image A).
- Has 4 major architectural patterns: micropapillary (image B), cribriform, tufted (image C) or flat.
- Nuclei often show stratification.
- Has nuclear features similar to cancer.
- Unlike cancer, contains basal cell layer either continuous or discontinuous (remember non cancerous glands always has basal cells).
- Immunohistochemistry: like in cancer AMACR is overexpressed, but unlike cancer basal cell markers (HMWK and p63)+ (image D).
- Median risk of cancer following diagnosis of high grade PIN is 21%.
- Presence of multifocal (>3) or bilateral HGPIN or associated with ASAP has higher risk for subsequent cancer.
- Current recommendation is to repeat biopsy if HGPIN is identified in needle biopsy without cancer.
- DDX: intraductal carcinoma (intraductal spread by cancer) of the prostate, which also has basal cells, high-grade secretory cells, and similarly has both AMACR and basal cell markers positivity.
- Unlike HGPIN, intraductal carcinoma has larger expansile glands and neoplastic cells span the entire lumen.
National Institute of Medical Coding
Contact No 09494833322





Comments
Post a Comment